Serotonin link upended
 New findings could change the understanding of how the gut communicates with the brain, and potentially alter the way antidepressants and other drugs are used.
New findings could change the understanding of how the gut communicates with the brain, and potentially alter the way antidepressants and other drugs are used.
A study, based on animal research, has explored the complex pathways between the brain and the gut, known as the gut-brain axis.
It found that the communication between the gut and the brain, particularly involving serotonin, occurs through diffusion rather than direct synaptic connections.
“The gut-brain axis consists of complex bidirectional neural communication pathway between the brain and the gut, which links emotional and cognitive centres of the brain,” says Flinders University's Professor Nick Spencer.
“As part of the gut-brain axis, vagal sensory nerves relay a variety of signals from the gut to the brain that play an important role in mental health and wellbeing.
“The mechanisms by which vagal sensory nerve endings in the gut wall are activated has been a major mystery but remains of great interest to medical science and potential treatments for mental health and wellbeing.”
The research focused on the activation mechanisms of vagal sensory nerve endings in the gut wall by serotonin - a crucial neurotransmitter and hormone implicated in a myriad of bodily functions, including mental health and depression.
Contrary to prior beliefs that enteroendocrine cells (EECs) in the gut wall made direct synaptic connections with the sensory nerve endings of the vagus nerve, this study discovered that communication between EECs and vagal sensory nerve endings occurs via diffusion.
“This is a major discovery for our understanding of gut-brain communication which has profound implications for drug developments, treatments of anxiety and depression and other digestive problems such as irritable bowel symptom (IBS), all of which involve serotonin in some way,” Professor Spencer said.
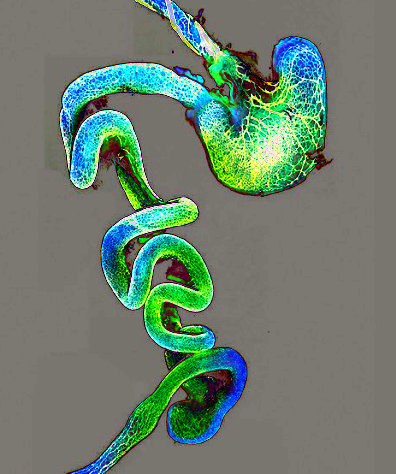
The study employed advanced anterograde neuronal tracing techniques to map the spatial relationships between serotonin-containing EECs and vagal nerve endings in the mouse colon.
Findings indicated that the mean distances between these entities were significantly greater than previously assumed, debunking the theory of synaptic transmission as the primary mode of communication.
“The absence of any close physical contacts between serotonin-containing EECs and vagal nerve endings in our studies leads to the inescapable conclusion that the mechanism by which serotonin activates the sensory nerve endings of the vagus nerve is by diffusion,” Professor Spencer said.
This research not only challenges existing paradigms about the gut-brain communication mechanism but also opens new avenues for the development of treatments for mental health conditions and digestive disorders.
The implications for the future of drug development and the therapeutic targeting of the gut-brain axis are vast, signalling a significant shift in how mental health and well-being might be approached scientifically and clinically in the future.








 Print
Print